Cancer screening protocols are structured approaches used by healthcare providers to detect certain types of cancer before a person exhibits any symptoms. For concerns related to the upper gastrointestinal (GI) tract, which includes the esophagus, stomach, and the first part of the small intestine, evaluation may be part of a broader health management plan. One procedure that may be referenced within these clinical pathways is the EGD.
What Is EGD?
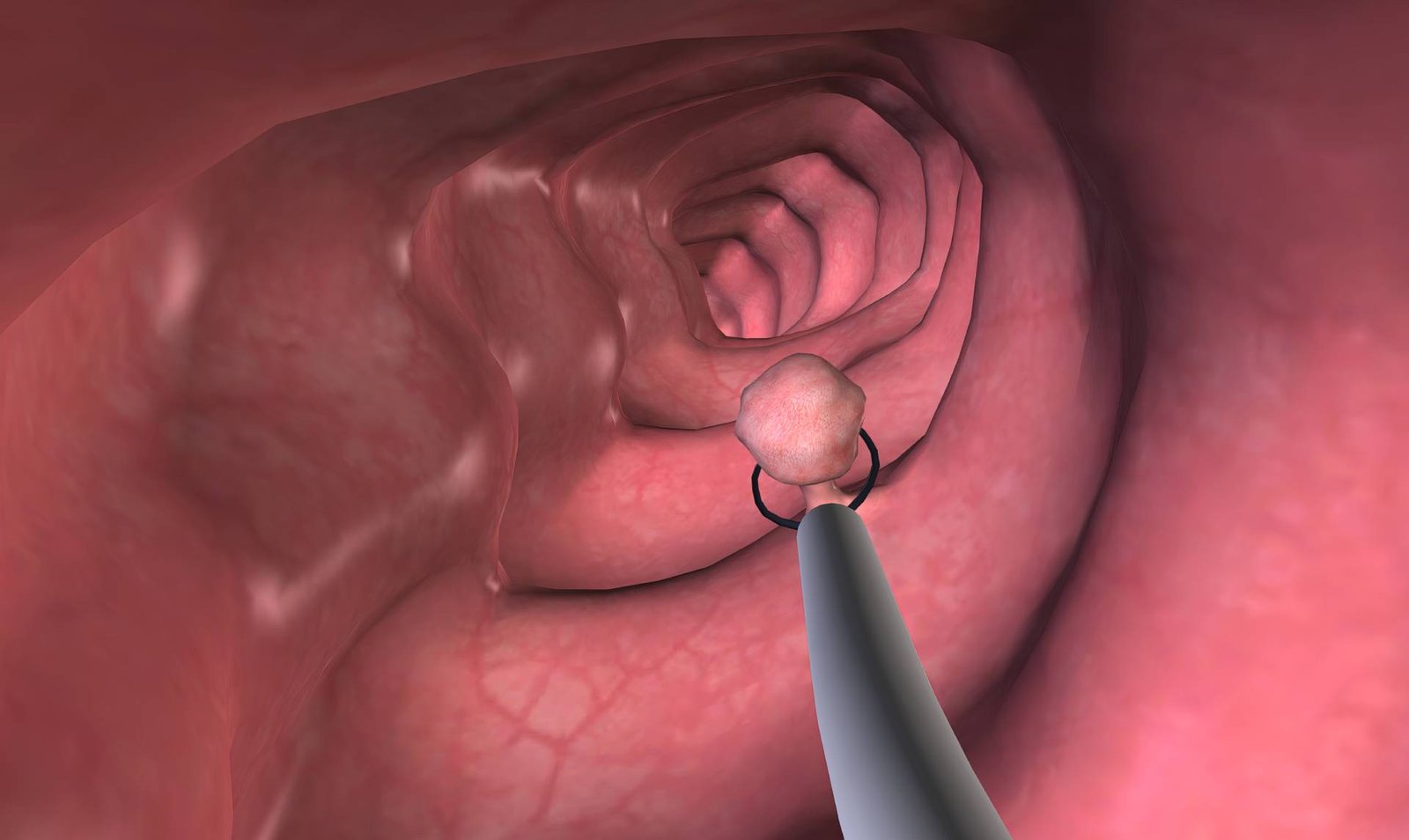
Esophagogastroduodenoscopy, commonly known as an EGD, is a medical procedure performed on an outpatient basis. It involves the use of an endoscope, which is a thin, flexible tube equipped with a camera at its tip. A trained physician, typically a gastroenterologist, guides the endoscope through the mouth, down the esophagus, into the stomach, and finally into the duodenum, which is the initial segment of the small intestine.
This process allows the physician to perform a direct visual examination of the lining of these organs. The camera transmits images to a monitor, enabling the clinician to observe the tissue surfaces in detail. The physician can document any variations in color, texture, or structure that are observed. This procedure serves as a method for direct visualization and documentation of the internal surfaces of the upper GI tract.
What Is It For?
A healthcare provider may use an EGD for several clinical reasons. It is often employed to investigate persistent upper GI symptoms that have not responded to initial treatments. Such symptoms can include recurring heartburn, difficulty swallowing, unexplained abdominal pain or bloating, and persistent nausea or vomiting. The procedure can also be used for the follow-up of previously diagnosed conditions, such as GERD or peptic ulcers.
During an EGD, a physician can obtain small tissue samples, a process known as a biopsy. These samples can be sent to a laboratory for pathological analysis. When clinical guidelines identify specific populations as having a higher potential for certain conditions, information from an EGD can contribute to their overall surveillance pathway. The procedure provides visual data and allows for tissue sampling, which can aid in documenting any changes.
What Should You Expect?
The EGD process typically begins after a consultation and scheduling with a gastroenterology office. You will receive specific instructions on how to prepare for the procedure, which usually includes a period of fasting. This means you will not be able to eat or drink for several hours beforehand to make sure the stomach is empty for a clear view.
On the day of the procedure, a nurse will likely place an intravenous (IV) line in your arm. This is used to administer a sedative medication. The sedation helps you relax and remain comfortable. Once you are sedated, the physician will gently insert the endoscope through your mouth and guide it through the upper digestive tract.
The examination itself is usually brief. If the physician observes areas that require further examination, they may perform biopsies to investigate the condition. After the procedure is complete, you will be moved to a recovery area to rest as the sedation wears off. Because of the lingering effects of the sedative medication, you may not be able to drive. It is helpful to arrange for a responsible adult to take you home.
Confer With a Specialist
An EGD is one of many procedures available within comprehensive healthcare programs. If you have questions or concerns about your digestive health, or if you would like to determine whether an evaluation is suitable for you, consulting a specialist is the appropriate course of action. A gastroenterologist can provide personalized guidance based on your unique health profile and explain the benefits and risks associated with any recommended procedure.

Leave a Reply